A Patient's Guide to Adult Metacarpal Fractures of the Hand
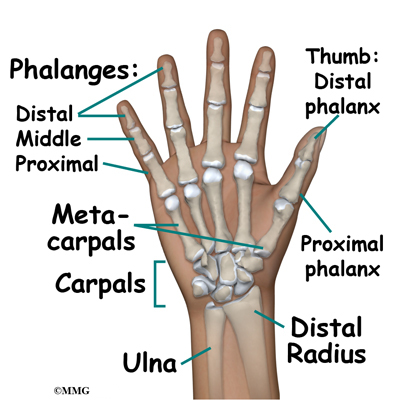
Anatomy
The metacarpals are the five bones of the hand that connect the carpal bones(wrist)to the proximal phalanges (fingers). Because of the special role the thumb plays in grasping, fractures of the thumb metacarpal are a bit different from the finger metacarpals and will be discussed separately in another document. The four finger metacarpals are tubular bones; the distal end (far end) is a round knob that forms a joint with a finger. These joints are commonly referred to as your knuckles. The proximal end (near end) of each bone forms a joint with one or more carpal bones. While the distal knuckle (metacarpophalangeal) joint has a great deal of motion, the proximal carpometacarpal joint has very little.
Signs and Symptoms
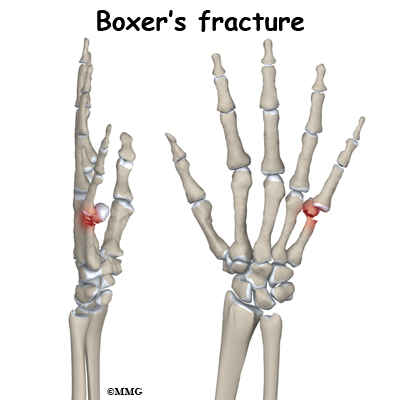
A metacarpal fracture can occur in a multitude of ways: a fall on the outstretched hand, a crushing injury, or hitting an object with your fist. Fractures of the metacarpal of the little finger are common after punching something (or someone) with a fist; they are even named a Boxer's fracture. There is usually immediate pain and swelling in the hand. You may also see that the hand is deformed. It is common to see a bump over the back of the hand where the fracture is located and angulated (or bent). If the fracture involves the metacarpal head (knob at the distal end of the bone) the knuckle may have seemed to disappear. Motion is painful; you will probably not be able to grip with the fingers due to pain.
Evaluation
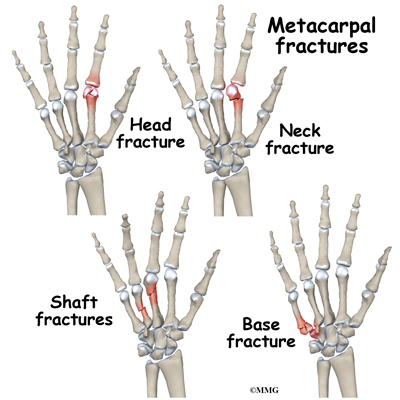
The primary goal of the clinical evaluation of a metacarpal fracture is to determine the pattern of the fracture. Based on the fracture pattern, your surgeon will need to decide if 1) the fracture is in stable alignment and can be simply protected in a cast or brace until it heals, 2) the fracture pattern can be reduced (or manipulated) to a stable alignment without surgery and held with a cast or brace until it heals, or 3) surgery will be necessary to align the fracture fragments and fix the fragments with some combination of metal pins, metal plates, and metal screws. The fracture is evaluated by taking several x-rays of the hand.
Treatment
Many metacarpal fractures do not require surgery. The metacarpals for the middle and ring finger are the least likely to require surgery because the other intact metacarpals on both sides form a natural splint that keeps the broken metacarpal fragments from displacing, rotating, or angulating too much. The proximal carpometacarpal joint of the little finger has much more motion than the other three. This means that more displacement and angulation after healing can be tolerated and not affect the function of the hand. The index metacarpal is the most likely to require surgery to restore the alignment of the fracture fragments because relatively small changes in the alignment can affect the function of the hand - and there is only one adjacent metacarpal to help stabilize the fragments through the natural splinting.
Nonsurgical

If your surgeon decides that the fracture can be treated without surgery, then a decision must be made whether to simply protect the fracture in a splint or cast until it heals or attempt better alignment of the fracture. If your surgeon decides that the fragments should be manipulated (moved) into alignment, then a closed reduction will be performed. To perform a closed reduction, a local anesthetic block is used to numb the hand around the fracture. Once the fracture is no longer painful, the surgeon will use a combination of pulling and pushing to align the fracture fragments into an acceptable position. A padded splint is usually applied that will support the wrist, hand, and affected fingers. Most fractures of the metacarpals heal enough in three or four weeks to remove the rigid splint and begin gentle, protected range of motion. X-rays will be taken frequently to make sure that the fracture remains in alignment. Once your surgeon thinks that the fracture has healed, the cast or fracture brace is discontinued and you will work with a physical therapist to regain the motion and strength in the arm and hand.
Surgery
A metacarpal fracture may require surgery. If your surgeon makes the assessment that the fracture will NOT give you good hand function without surgery, surgical treatment will be recommended. If the fracture cannot be held in acceptable position with a cast or fracture brace and the fragments begin to separate, surgery may be suggested after several days or weeks of attempting nonsurgical treatment. Surgical treatment of metacarpal fractures can be performed in several ways: metal pins placed through the skin and into the fracture fragments to hold them in place or a combination of small metal screws with or without a small metal plate along the side of the bone.
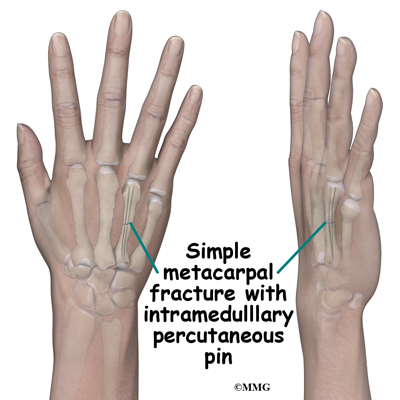
Surgical treatments that range from relatively simple to more complex may be considered depending on the fracture pattern. Simple fracture patterns may be treated by placing metal pins through the skin and into the bone fragments to hold the fragments in position as they heal. While you are in the operating room these pins are inserted with the aid of a special X-ray machine called a fluoroscope. The fluoroscope allows the surgeon to see an X-ray image of the bones on a television monitor and guide the placement of the pins by viewing this image. This type of surgery may be done as an outpatient.
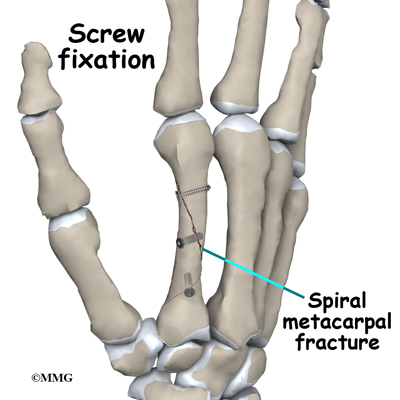
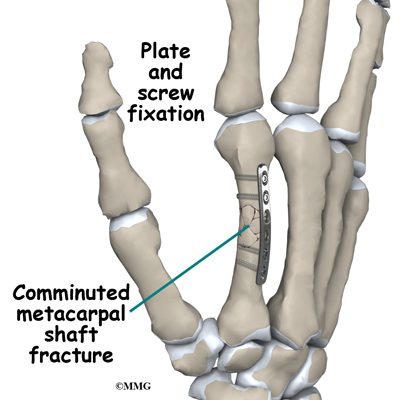
Some metacarpal fractures require Open Reduction and Internal Fixation (ORIF) using small metal screws or a metal plate and screws. This type of treatment allows the fracture fragments to be restored as close to their normal position as possible and held there until healing occurs. This type of treatment may be necessary to restore the alignment as close as possible. ORIF usually requires an incision on the dorsal (back) side of the hand.
Complications
Nearly all fractures can result in damage to nerves and blood vessels; but this is a rare complication of most metacarpal fractures. Because metacarpal fractures are sometimes associated with punching someone, lacerations (cuts in the skin) can occur over the knuckles as part of the injury. When these lacerations are caused by human teeth, there is a great risk of serious infection complicating the fracture. This will usually require immediate surgery to cleanse the wound, the knuckle joint and possibly the fracture to reduce the risk of serious infection.
Chronic Regional Pain Syndrome (CRPS) is another uncommon, but serious, potential complication of metacarpal fractures. The cause of this problem is unknown; CRPS can occur anywhere in the body but is more common in the extremities - the arm and leg. Following a fracture of the hand, a few patients have had their arm and hand become immediately swollen and intensely painful. The nervous system of the extremity seems to become deranged. Treatment consists of medications to control the nerve pain, injections to block the sympathetic nerves to the extremity in an attempt to stop the process and physical therapy to regain function as soon as possible. CRPS can be very frustrating and become a chronic condition; luckily, the complication is rare.
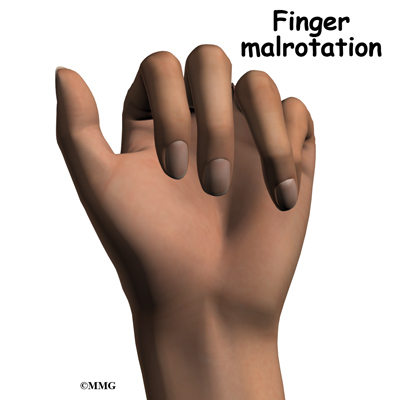
The fracture fragments may fail to heal; this is referred to as a nonunion. The fracture fragments may also heal in an unacceptable alignment; this is called malunion. If either of these complications occur, the result may be pain, loss of strength and decreased function of the hand and fingers. A second operation may be needed to treat the complication.
Rehabilitation
The prognosis for metacarpal fractures is generally excellent. The fingers become stiff very fast after being immobilized - whether they are injured or not. Most hand surgeons try to limit the time that the fingers are immobilized and begin physical therapy as soon as possible to prevent stiffness from occurring. Rehabilitation will begin once your surgeon feels that the fracture is stable enough to begin regaining the range of motion in your wrist, hand and fingers. If surgery has been required, the rehabilitation program will be modified to protect the fixation of the fracture fragments. Your surgeon will communicate with your physical therapist to make sure that your rehabilitation program does not risk causing the fixation to fail. If the surgeon feels that the fixation is very solid, you may be able progress your program quickly; if the fixation is not so solid, the speed at which you progress may need to be slowed until more healing occurs.
|
