A Patient's Guide to Labral Tears of the Hip
Introduction
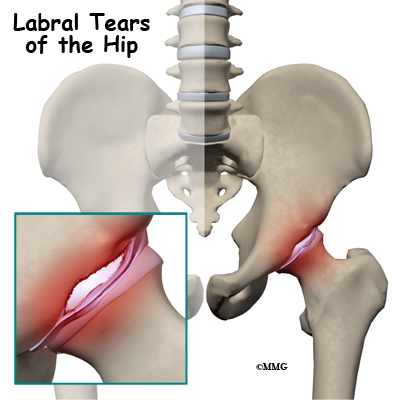
Acetabular labrum tears (labral tears) can cause pain, stiffness, and other disabling symptoms of the hip joint. The pain can occur if the labrum is torn, frayed, or damaged. Active adults between the ages of 20 and 40 are affected most often, requiring some type of treatment in order to stay active and functional. New information from ongoing studies is changing the way this condition is treated from a surgical approach to a more conservative (nonoperative) path.
This guide will help you understand
- what parts of the hip are involved
- how the condition develops
- how doctors diagnose the condition
- what treatment options are available
Anatomy
What parts of the hip are involved?
The acetabular labrum is a fibrous rim of cartilage around the hip socket that is important in normal function of the hip. It helps keep the head of the femur (thigh bone) inside the acetabulum (hip socket). It provides stability to the joint.
Our understanding of the acetabular labrum has expanded just in the last 10 years. The availability of high-power photography and improved lab techniques have made it possible to take a closer look at the structure of this area of the hip.
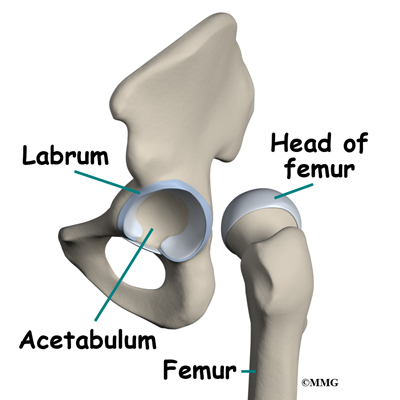
The labrum is a piece of connective tissue around the rim of the hip socket (acetabulum). It has two sides: one side is in contact with the head of the femur, the other side touches and interconnects with the joint capsule. The capsule is made up of strong ligaments that surround the hip and help hold it in place while still allowing it to move in many directions,
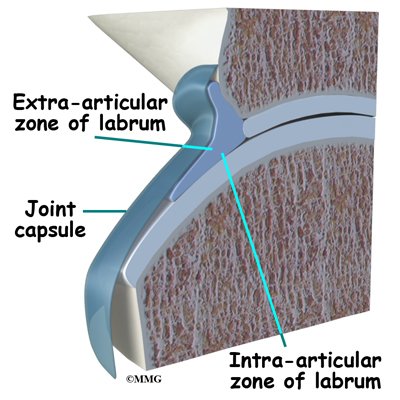
Finding out that there are two separate zones of the labrum was an important discovery. The extra-articular side (next to the joint capsule) has a good blood supply but the intra-articular zone (next to the joint) is mostly avascular (without blood). That means any damage to the extra-articular side is more likely to heal while the intra-articular side (with a very poor blood supply) does not heal well after injury or surgical repair.
The labrum helps seal the hip joint, thus maintaining fluid pressure inside the joint and providing the overall joint cartilage with nutrition. Without an intact seal, the risk of early degenerative arthritis increases. A damaged labrum can also result in a shift of the hip center of rotation. A change of this type increases the impact and load on the joint. Without the protection of the seal or with a hip thatís off-center, repetitive motion can create multiple small injuries to the labrum and to the hip joint. Over time, these small injuries can add to wear and tear in the hip joint.
Causes
How does this condition develop?
It was once believed that a single injury was the main reason labral tears occurred (running, twisting, slipping). But with improved radiographic imaging and anatomy studies, itís clear now that abnormal shape and structure of the acetabulum, labrum, and/or femoral head can also lead to the problem.
Injury is still a major cause for labral tears. Anatomical changes that contribute to labral tears combined with repetitive small injuries lead to a gradual onset of the problem. Athletic activities that require repetitive pivoting motions or repeated hip flexion cause these type of small injuries.
What are these ďanatomical changesĒ? The most common one called femoral acetabular impingement (FAI) is a major cause of hip labral tears. With FAI, there is decreased joint clearance between the junction of the femoral head and neck with the acetabular rim.
Related Document: A Patient's Guide to Femoroacetabular Impingement
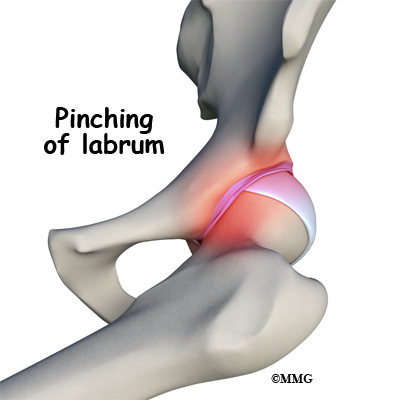
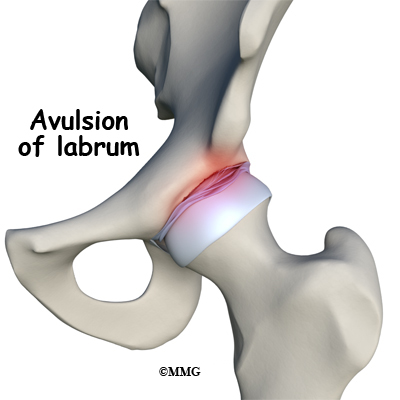
When the leg bends, internally rotates, and moves toward the body, the bone of the femoral neck butts up against the acetabular rim pinching the labrum between the femoral neck and the acetabular rim. Over time, this pinching, or impingement, of the labrum causes fraying and tearing of the edges. A complete rupture is referred to as an avulsion where the labrum is separated from the edge of the acetabulum where it normally attaches.
Changes in normal hip movement combined with muscle weakness around the hip can lead to acetabular labrum tears. Other causes include capsular laxity (loose ligaments), hip dysplasia (shallow hip socket), traction injuries, and degenerative (arthritic) changes associated with aging. Anyone who has had a childhood hip disease (such as Legg-Calvť-Perthes disease, hip dysplasia, slipped capital femoral epiphysis) is also at increased risk for labral tears.
Related Document: A Patient's Guide to Perthes Disease
Related Document: A Patient's Guide to Developmental Dysplasia of the Hip in Children
Related Document: A Patient's Guide to Slipped Capital Femoral Epiphysis
Symptoms
What does this condition feel like?
Pain in the front of the hip (most often in the groin area) accompanied by clicking, locking, or catching of the hip are the main symptoms reported with hip acetabular labral tears. Joint stiffness and a feeling of instability where the hip and leg seem to give away are also common. The pain may radiate (travel) to the buttocks, along the side of the hip, or even down to the knee.
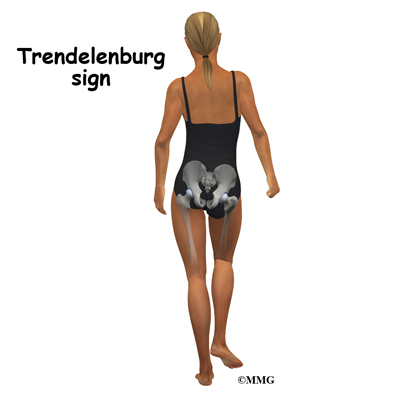
Symptoms get worse with long periods of standing, sitting, or walking. Pivoting on the involved leg is avoided for the same reason (causes pain). Some patients walk with a limp or have a positive Trendelenburg sign (hip drops down on the right side when standing on the left leg and vice versa).
The pain can be constant and severe enough to limit all recreational activities and sports participation.
Diagnosis
How will my doctor diagnose this condition?
The history and physical examination are the first tools the physician uses to diagnose hip labral tears. There may or may not be a history of known trauma linked with the hip pain. When there are anatomic and structural causes or muscle imbalances contributing to the development of labral tears, symptoms may develop gradually over time.
Your doctor will perform several tests. One common test is the impingement sign. This test is done by bending the hip to 90 degrees (flexion), turning the hip inward internal rotation) and bringing the thigh towards the other hip (adduction).
Making the diagnosis isnít always easy. In fact, this problem is frequently misdiagnosed at first. Thatís because there are many possible causes of hip pain. The pain associated with labral tears can be hard to pinpoint. Your doctor must rely on additional tests to locate the exact cause of the pain. For example, injecting a local anesthetic agent (lidocaine) into the joint itself can help determine if the pain is coming from inside (versus outside) the joint.
X-rays provide a visual picture of any changes out of the ordinary of the entire structure and location of the hip position. Magnetic resonance imaging (MRI) gives a clearer picture of the soft tissues (e.g., labrum, cartilage, tendons, muscles).
One other test called a magnetic resonance arthrography (MRA) is now considered the gold standard for diagnosis. Studies show that MRA is highly sensitive and specific for labral tears. This test may replace arthroscopic examination as the main diagnostic tool. Arthroscopic examination is still 100 per cent accurate but requires a surgical procedure.
With MRAs, contrast dye (gadolinium) is injected into the hip joint. Any irregularity in the joint surface will show up when the dye seeps into areas where damage has occurred. MRAs give the surgeon an excellent view of the location and extent of the tear as well as any bony abnormalities that will have to be addressed during surgery.
Treatment
What treatment options are available?
In the past, when arthroscopic surgery was the only way to confirm the presence of a labral tear, the surgeon would just go ahead and remove the torn edges or pieces during the arthroscopic examination procedure. However, studies over the years have called this approach into question. With removal of the labrum, changes in the way the hip functioned, increased friction of the joint, and increased load on the joint led to degenerative changes and osteoarthritis.
Surgeons stopped cutting out the torn labrum and started repairing it instead. Physical therapists started doing studies that showed strengthening muscles and resolving issues of muscle imbalances could reduce the need for surgery with the traditional risks (e.g., bleeding, infection, poor wound healing, negative reactions to anesthesia).
More efforts are being made now to manage labral tears with conservative (nonoperative) care. This is a possibility most often when there are no symptoms of labral pathology. Patients with confirmed labral tears but who have normal hip anatomy or only mild changes in the shape and structure of the hip may also benefit from conservative care.
Nonsurgical Treatment
Physical therapy will probably be suggested. Your physical therapist will carry out an examination of joint motion; hip, trunk, and knee muscle strength; posture; alignment; and gait/movement analysis (looking at walking/movement patterns). A plan of care is designed for each patient based on his or her individual factors and characteristics.
Nonoperative care starts with activity modification. You should avoid pivoting on the involved leg and avoid prolonged periods of weight-bearing activities. You physical therapist will work with you to on strengthen your hip muscles, restore normal neuromuscular control, and improve your posture. All of these things can improve your hip function and reduce your pain.
Tight muscles around the hip can contribute to pinching between the femoral head and acetabulum in certain positions. A program of flexibility and stretching exercises wonít change the bony abnormalities present but can help lengthen the muscles and reduce contact and subsequent impingement.

A special strap called the SERF strap (SERF means Stability through External Rotation of the Femur) made of thin elastic may be applied around the thigh, knee, and lower leg to pull the hip into external rotation. The idea is to use the strap to improve hip control and leg movement during dynamic activities. It is important to strengthen the muscles at the same time to perform the same task and avoid depending on external support on a long-term basis.
Some patients may also benefit from intra-articular injection with cortisone. Cortisone is a very potent antiinflammatory medication. Injection into the hip joint may reduce the symptoms of pain for several weeks to months.
Surgery
Arthroscopy is commonly used to repair the torn labrum. The arthroscope is a small fiber-optic tube that is used to see and operate inside the joint. A TV camera is attached to the lens on the outer end of the arthroscope. The TV camera projects the image from inside the hip joint on a TV screen next to the surgeon. The surgeon actually watches the TV screen (not the hip) while moving the arthroscope to different places inside the hip joint and bursa.
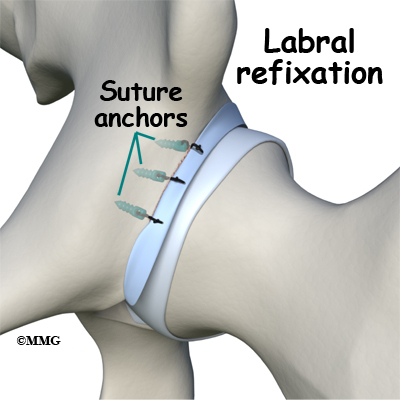
During this procedure, your surgeon will trim the torn and frayed tissue around the acetabular rim and reattach the torn labrum to the bone of the acetabular rim. This procedure is called labral refixation. Each layer of tissue is sewn back together and reattached as closely as possible to its original position along the acetabular rim.
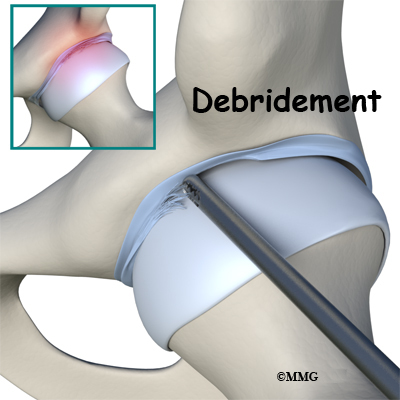
When repair is not possible, then debridement of the torn labral tissue may be necessary. Debridement simply means that the torn or weakened portions of the labrum are simply removed. This prevents the torn fragments from getting caught in the hip joint and causing pain and further damage to the hip joint.
In some cases, open treatment of femoroacetabular impingement and/or correction of bone abnormalities are required. These procedures are much more involved and usually will require a stay of several days in the hospital.
Rehabilitation
What should I expect after treatment?
Nonsurgical Rehabilitation
The goal of conservative management is to relieve pain and improve function by correcting muscle strength imbalances. When both legs have nearly equal strength, it is possible to resume a full and normal level of all activities as long as there is no pain during any of those movements or activities./
For the young or active adult, this includes activities of daily living as well as recreational and sports participation. Older adults experiencing labral tears from degenerative arthritis may expect to be able to resume normal daily functions, but may still find it necessary to limit prolonged sitting or standing positions.
After Surgery
Correction of the problem causing labral tears can result in improved function and pain relief. The hope is that early treatment can prevent arthritic changes but long-term studies have not been done to proven this idea.
Recovery after surgery needed to address hip labral tears usually takes four to six months. In other words, patients can expect to resume normal activities six months after surgery. Many athletes or highly active adults find this time frame much too long for their goals and preferences.
Patients who follow the recommended rehab plan of care respond well to progression of the exercises and seem to recover faster. Discharge from rehab takes place when the patient can perform all exercises with good form and without pain or other symptoms. Any repeat episodes of groin and/or hip pain must be reported to the orthopedic surgeon for evaluation right away.
|
