A Patient's Guide to Chronic Pain Management
Introduction
According to the National Center for Health Statistics chronic pain health care costs and lost productivity has reached nearly $100 billion a year. It affects approximately 76.2 million people - more individuals than diabetes, heart disease and cancer combined.
The primary goals in chronic pain management are to assess, understand and treat your pain condition.
This sounds simple. It is not simple or easy. The process requires a great deal of time and effort on both the part of the pain management team and you.
This guide will help you understand
- what chronic pain is
- what pain management is
- how chronic pain is managed
- what you can expect from pain management
What is chronic pain?
Chronic pain is sometimes defined officially as pain lasting more than 6 months. It may also be accurate to define chronic pain as pain that has no clear end in sight. It may be something that you will have to learn to live with - or around.
Anyone who has lived with chronic pain, or has treated patients with chronic pain, eventually comes to the understanding that the chronic pain is a disease in itself, regardless of what is causing the pain. It is this disease - chronic pain - that pain management specialists treat.
This does not mean that the team will ignore what is causing your pain. The first goal is to assess your pain. This means that your healthcare provider must try to determine, if possible, what is causing your pain..
The first question that should be asked is: "Does the pain have a source that can be eliminated by doing something to you - such as a medical treatment or surgery?"
Usually, the doctors that you have seen before you arrive at a pain management center have already done this. They refer you to the pain management center because they have not found anything that will reliably eliminate your pain. The pain management team will start from scratch and review all the tests and imaging studies that have been done and examine you. Sometimes the pain specialist may uncover new things or make new diagnoses. Usually they do not.
Once your pain management specialists have satisfied themselves that there is no reliable way to eliminate your pain through a medical treatment or surgery, they will begin the process of understanding your pain. This is a complex process. It does not end as long as you have the pain. The pain management team will constantly reevaluate what they think about your pain, how it is affecting you and what is needed to change the approach to helping you live with your pain.
Understanding your pain and treating your pain go hand in hand. How you respond to certain treatments gives your pain specialists a better understanding of your pain. They probably will not get the right, or best, combination on the first try - or the second. But they will continue to work with you to refine the treatment plan so that you get the best plan that can be can offered. Understanding your pain is a never ending process - for you or for your healthcare providers. Have patience both with yourself and with your pain management team.
In the majority of chronic pain patients, the sensation of pain will NOT be eliminated. BUT, with treatment you can drastically change how much the pain affects your life. Chronic pain is a disease that can be managed effectively. You should expect your pain management team to work with you and your primary care provider to effectively manage your chronic pain condition with all of the expertise and tools available as long as you need help.
Once the process of creating a treatment plan with you begins, there are many different options that can be explored. An important thing for you to realize is that these options are divided into two groups:
- Things people do to you
- Things you learn to do for yourself
Each of these approaches are important and have value in treating your pain. The goal is to find a balance where you are in control of as much of your treatment plan as possible - while you minimize the treatment options that require something to be delivered that is controlled by someone else. This situation just makes more sense in the long run - because it puts you more in control of managing your pain. It's cheaper, requires less time spent in providers' offices and ultimately it is more effective.
Most chronic pain patients do require some passive modalities -- "things people do to you" - such as medications, massage and injections to deaden the pain at times. Early on this seems to be more important as you learn the skills that will allow you to move beyond dependence on some of these passive modalities. Remember, the main goal is to help you manage your pain in a way that is effective for you. If that requires some passive modalities, then so be it.
Things People Do To You
In our current healthcare culture, we are used to going to see a practitioner when we are ill and saying, "Fix it!" Most practitioners are quite willing to try to do just that - give you a prescription medication or suggest a surgical procedure that is designed to cure or fix your problem. Our expectation is that everything can be fixed if we just find the real problem and match this with the real cure.
Pain doesn't necessarily work that way. In fact, most things in healthcare don't really work that way, but we all pretend they do - patients and doctors alike. With the exception of things like appendicitis and broken bones, most healthcare conditions have lifelong effects that must be dealt with sooner or later. In chronic pain, it just happens sooner rather than later. Quit fooling yourself early and get on with the business of managing chronic pain.
Most of the passive modalities in the category of "things people do to you" are temporary fixes rather than cures. They are useful in managing symptoms while you and your providers work on the category of "things you learn to do for yourself". That is not to say that many of these things people do to you are not beneficial. Some may control your symptoms for years. Some may need to be returned to and used even years from now when you are having a flare up of pain. Just don't think of them as a "cure". They are tools in your toolbox. Use the right tool for the job. If a small tap is needed - don't use a sledgehammer.
Some of the more common things that fall into the "things people do to you" category are:
- Invasive interventions
- Medications
- Physical modalities
Invasive Interventions
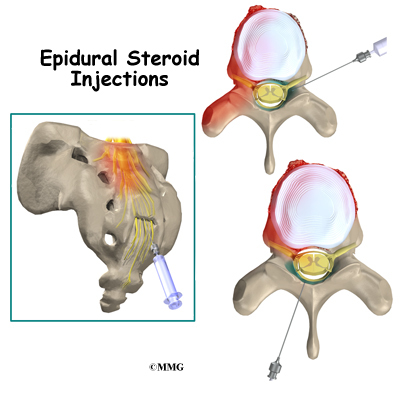
Invasive interventions are treatments that require surgery or some type of procedure that involves physically invading the body - such as an injection. Clearly, many surgical and invasive procedures are done to reduce or eliminate pain. Many are successful - some are not. You may already have had one or several invasive procedures. You may need more in the future.
Many of the patients in chronic pain management programs are not expecting any invasive procedures in the near future. This is usually because there are no procedures to recommend that have a reasonable chance of success. Your pain specialist never stops considering invasive interventions to help treat your pain because things constantly change. BUT, continuing to look for the ultimate cure can lead to delays in getting down to managing the chronic pain disease itself.
Medications
Medications treat the symptoms of chronic pain - not the disease itself. Nearly every patient with chronic pain will have the following symptoms at some point in their management program:
- Depression
- Sleep difficulty
- Anxiety
Medications can help control these symptoms to a degree. Medications alone are not the answer. Any medication treatment must be combined with other treatments. For example, many studies show that depression responds exceedingly well to exercise and psychotherapy - possibly better than to medications. The same is true for sleep difficulty and anxiety - both cannot be adequately treated with medications alone.
Anytime a medication is used for control of the symptoms of chronic pain, realize that you must weigh the side effects versus the benefits. All medications have side effects. No medications are risk free.
Narcotic pain medications are especially difficult to use due to the side effects of physical dependence and addiction. Chronic pain patients use narcotic medications frequently - but do so with a respect for the potential harm that they can cause. The real goal is to treat your pain effectively so that you do not need narcotic pain medications if possible. That is not always achievable.
Medications are one piece of the puzzle - not the total answer. The goal is to use the minimum amount of medication necessary to treat your pain. If that is a lot of medications then fine, if it is none, that's fine too. In general, the less medication the better.
Physical Modalities

Physical modalities include things like massage, acupuncture, ultrasound, TENS and chiropractic. These are treatments that require someone else to touch you, stick a needle in you or manipulate your body. In some cases (such as TENS), you need to attach yourself to some type of machine that does something to you. None of these things are necessarily bad or good. If they help relieve any of the symptoms of chronic pain, then they may be useful.
Unlike medications and invasive treatments, most of these modalities are relatively risk free. But, similar to medications, these modalities usually provide temporary relief. Pain specialists use these modalities frequently as part of a comprehensive symptom management program. The biggest risk in coming to rely more and more on these passive modalities for reducing symptoms is that you give up some control of your management program.
As is true in every aspect of managing chronic pain, reaching a balance is necessary.
Things You Learn To Do For Yourself
The things you learn to do for yourself to manage your chronic pain are the most important in the long run.
That bears repeating:
The things you learn to do for yourself to manage your chronic pain are the most important in the long run.
The more pain management skills you master, the more YOU control your chronic pain without relying on other people to do something to you or control your treatment. You become more empowered. You are in charge, not the healthcare provider.
Some of the more common things that fall into "the things you learn to do for yourself" category are:
- Ergonomics
- Exercise
- Mind body techniques
Ergonomics
Ergonomics is simply a fancy word for describing a relatively simple concept - how we use our bodies to interact with our physical surroundings. Learning about good ergonomics means learning how to get things done without aggravating your underlying condition and causing pain. It is amazing how many people come into a pain program who never realize how many things they do during the day are actually causing problems. Once they learn new ways of doing things and new ways to arrange their home and work environment, their pain decreases.
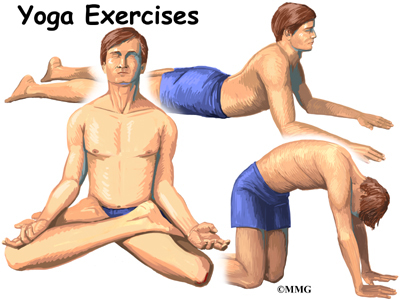
Exercise
Developing an exercise routine is critical in the management of chronic pain. You will not be able to effectively manage your pain without incorporating some form of exercise as part of your daily routine. This is not a one-size-fits-all approach to exercise. We realize that each patient is different, with a different set of physical problems that affect what type of exercise is reasonable. Everyone will have a different program designed specifically with their unique problems in mind.

Exercise will reduce many of the symptoms of chronic pain. Even small doses of regular exercise cause physiologic changes in the body chemistry that are beneficial. Exercise increases the body's internal pain killing chemicals called endorphins. These chemicals act just like morphine to reduce pain. Exercise is effective in reducing depression and can help burn off the excess adrenaline that causes anxiety. Most chronic pain patients find that they sleep much better when they begin a regular exercise program.
If you allow chronic pain to greatly reduce your activity level, deconditioning of muscles and ligaments occurs. Bones become weaker. Injury is more likely and pain actually increases. Moderate amounts of exercise will protect you from the effects of deconditioning and help you improve your ability to function.
Remember, the goal is not necessarily to become pain free, but to strike a balance between reducing pain and maintaining function. Some degree of discomfort is not necessarily a bad thing. Many people are afraid that discomfort means they are doing some type of damage to their body. That is not necessarily true. A bit of discomfort is warranted to maintain a higher level of function as long as you are not doing further damage. Doing nothing will certainly result in further damage to your body. Part of what you will be learning is how to tell when enough is enough.
Mind Body Techniques
Many of the symptoms of chronic pain disease are actually made much worse by our minds. The way we react to the sensation of pain is a combination of primitive reflexes (designed or evolved to protect us from harmful things) and learned behavior (not necessarily useful to us at all). For example, think about the muscle pain you might have when you have overdone your spring gardening. You know by experience that it is a simple muscle soreness and you are certain it will go away in a few days. You are not too concerned. You ignore it. It goes away.
Now imagine you wake up one morning with a pain for no good reason. It doesn't go away in a few days. You become concerned because you don't know what the pain MEANS. Is it serious? Does the pain mean I am damaging my body when I do things that make the pain worse? You become anxious. This releases chemicals in your body that increase the sensitivity of your nerves to the pain - the pain feels worse!
All of these changes occur at the subconscious level - so you are not necessarily aware of this change that comes over you. The result is that you are turning the volume up on your pain. Mind body techniques teach you how to turn down the volume on your pain. The pain song might still be playing in the background - but it's more like elevator music than hard rock.
Most mind body techniques try to tap into what we call physiologic quieting. The mind has a great deal of influence over the hormones and chemicals that are released when we are stressed. These are the chemicals that increase the volume of your pain. You can train yourself to reduce the release of these chemicals and turn down the volume. These are very powerful tools to have in your toolbox. No chronic pain management program will be successful without incorporating some of these mind body techniques.
|
